Medicaid, a healthcare safety net for low-income individuals, operates with unique eligibility criteria in each state. The Health Policy Institute of Ohio reports that as of 2025, more than 3 million Ohioans — more than 1 in 4 people in the state, are enrolled in Medicaid.
Ohio focuses on income thresholds and asset limits for categories like adults under 65, children, pregnant women, and seniors. Recent legislative updates, such as postpartum coverage extensions and routine redetermination processes, shape Ohio’s Medicaid structure.
We know Medicaid eligibility and managing assets can feel complicated, but that’s why we’re here. At Jarvis Law Office, based in Ohio, our one-time fee option helps you save money compared to ongoing life insurance costs. We also work closely with your financial advisor to ensure your plan fits your needs perfectly.
Key Takeaways
- Medicaid provides essential healthcare coverage for low-income individuals, including adults, children, pregnant women, seniors, and disabled individuals, with eligibility based on income and asset limits.
- Ohio has specific income and asset thresholds for Medicaid applicants and different Federal Poverty Level (FPL) requirements depending on the applicant’s category.
- Applying for Medicaid in Ohio is straightforward, with options to apply online, by phone, or in person at county agencies, but applicants must provide correct documentation to avoid delays.
- Recent legislative changes have impacted Medicaid enrollment, with over 867,000 Ohio residents losing coverage due to the reinstatement of eligibility redeterminations and new work requirements.
What is Medicaid?
Medicaid is a joint federal and state program offering health coverage to eligible low-income individuals. It covers critical services such as doctor visits, hospital stays, preventive care, and long-term care for vulnerable populations.
Who Does Medicaid Target in Ohio?
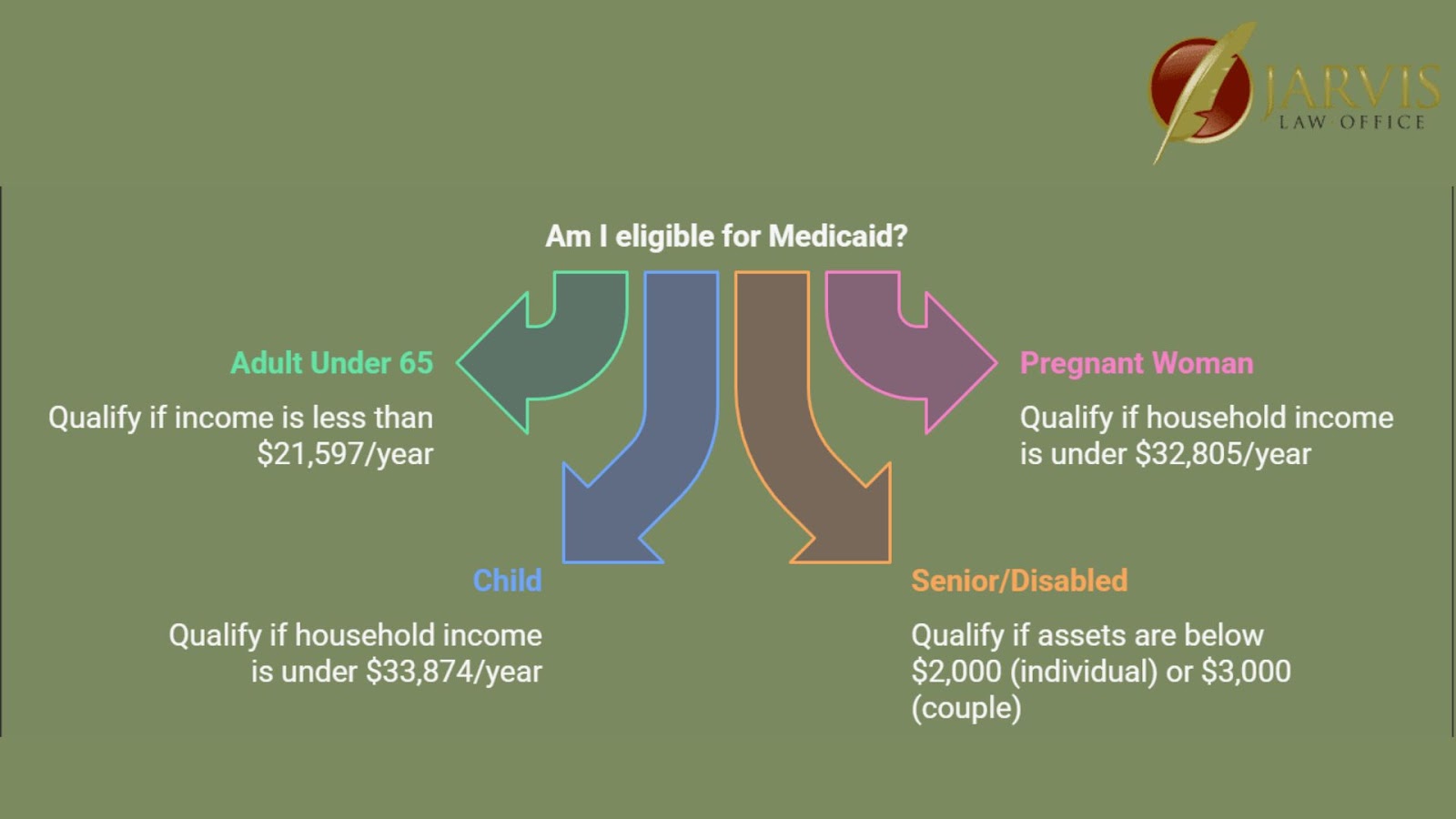
According to the Ohio Department of Medicaid, Medicaid targets specific groups, resulting in different income and asset limits.
Income Limits by Group
Eligibility for Medicaid in Ohio is primarily based on household income as a percentage of the Federal Poverty Level (FPL). Below are the key income limits:
Adults Under 65
- Income limit: 138% of FPL
- Approximate annual income: $21,597 for a single person
- Includes individuals without dependent children.
Pregnant Women
- Income limit: 205% of FPL
- Approximate annual income: $32,805 for a household of two
- Coverage extends throughout pregnancy and postpartum for eligible applicants.
Children
- Income limit: 211% of FPL
- Approximate annual income: $33,874 for a household of two
- Covers children under 19 years old, offering preventive and ongoing medical care.
Seniors and Disabled Individuals
- Income limit: Varies based on Supplemental Security Income (SSI) eligibility.
- Asset/resource threshold: $2,000 for individuals and $3,000 for couples.
Asset Limits for Special Groups
Certain Medicaid programs in Ohio impose strict asset limits in addition to income requirements. These include:
Nursing Home Medicaid
- In 2025, applicants must have assets below $2,000 and an income limit of $2,901/month.
- Covers long-term care, including nursing homes and community-based services.
Supplemental Security Income (SSI) Recipients
- Individuals receiving SSI automatically qualify for Medicaid.
- Asset limits remain the same: $2,000 for individuals and $3,000 for couples.
3 Ways to Apply for Medicaid in Ohio
Applying for Medicaid in the Buckeye state is designed to be straightforward and accessible. Residents can choose either of these options to apply for Medicaid:
1. Online Applications via the Ohio Benefits Website
The Ohio Benefits platform offers a user-friendly portal for applications. Applicants can create an account, check eligibility, and submit documents digitally.
2. Phone Application and Assistance
Applicants can call the Medicaid helpline to receive support. This option is ideal for those who prefer live assistance. Counties, such as those near Cleveland or Columbus, have dedicated service representatives.
3. In-Person Application at County Agencies
Residents of areas like Franklin County or Cuyahoga County can visit local Job and Family Services offices. In-person applications allow direct assistance with documentation and questions.
What Documents Do You Need for Medicaid Applications?
For a smooth process, applicants should prepare these documents:
- Proof of Identity: State-issued ID, birth certificate, or driver’s license from Ohio.
- Income Verification: Pay stubs or employer letters.
- Immigration Status (if applicable): Non-citizens must provide documentation of lawful status.
- Residency Verification: Utility bills or rental agreements showing residency in the Midwest region.
Common Mistakes to Avoid When Applying for Medicaid
Individuals applying for Medicaid in this state should avoid:
- Incomplete Forms: Missing sections may delay approval.
- Incorrect Income Reporting: Use accurate figures to prevent rejection.
- Not Responding to Communications: Be prompt in replying to Job and Family Services inquiries.
Impact of Recent Legislation on Ohio Medicaid
Ohio’s Medicaid program has undergone significant changes due to recent legislative updates. According to the Ohio Department of Medicaid, the termination of the continuous enrollment provision resulted in over 867,000 residents losing Medicaid coverage.
Meanwhile, the introduction of a work requirement for certain enrollees may further impact eligibility for adults under 65. Despite these challenges, Ohio’s Medicaid expansion has successfully extended coverage to approximately 2.9 million residents, demonstrating the program’s broad reach.
Additionally, Ohio’s reliance on federal funding—accounting for 73% of Medicaid’s revenue—shows its critical role in sustaining the program. Efforts like the Next Generation Managed Care Initiative, which brings on new partners, programs and services to Medicaid, continue to focus on improving service across the state.
Extended Postpartum Coverage and Its Significance
In a significant stride toward improving maternal health, Ohio extended its postpartum Medicaid coverage from 60 days to one year after childbirth in April 2022. This extension is an important step in reducing health disparities, providing approximately 44,000 women with essential services annually.
These services include mental health support, preventive care, and chronic condition treatment. Extended postpartum coverage aims to counter Ohio’s high rates of maternal mortality and morbidity, particularly among women of color.
It forms part of a broader initiative to improve maternal health outcomes and guarantee continuity of health coverage during the critical shift from pregnancy to motherhood.
Medicaid Eligibility Redetermination in Ohio

During the pandemic, Ohio’s Medicaid beneficiaries benefited from continuous coverage without needing to requalify. But in April 2023, the state reinstated its eligibility redetermination process, requiring recipients to verify their eligibility or risk losing coverage.
According to the Ohio Department of Medicaid, this change was part of a nationwide shift as pandemic-related policies came to an end.
States, including Ohio, were given 14 months to complete the process. By spring 2024, over 867,000 residents had been disenrolled due to no longer meeting eligibility requirements or failing to respond to verification notices.
However, individuals losing Medicaid had options, including transitioning to healthcare marketplace plans or other assistance programs.
The Ohio Department of Medicaid emphasizes the importance of promptly responding to eligibility notices to prevent unnecessary disenrollment and allow for continuous healthcare access.
Frequently Asked Questions
1. What Is the Income Limit for Medicaid in Ohio?
The income limit is 138% of the Federal Poverty Level (FPL), roughly $21,597 annually for a single person.
2. How Do I Find Out if I Am Eligible for Medicaid in Ohio?
Check eligibility by comparing your income to Ohio’s Medicaid limits on the Ohio Benefits website or contact your local County Job and Family Services office.
3. What Disqualifies You From Medicaid?
You can be disqualified for:
- Income exceeding limits.
- Assets surpassing thresholds.
- Non-compliance with documentation.
- Failing to meet care requirements or lawful immigration status.
Ready to Secure Your Family’s Future?
At Jarvis Law Office, we’re dedicated to helping Ohio families protect their assets, avoid probate, and simplify the Medicaid process. Our team is here to make sure you’re prepared for the future.
If you’re ready to take the next step, visit our contact page to connect with us. We’d love to answer your questions and help you create a plan that works for your family.